Do I really need the flu shot? And other questions to address this flu season
Flu viruses are common during fall and winter. In North America, the flu season usually lasts from October through February but can extend all the way through May. Flu activity usually peaks December through February.
Pharmacists, doctors, and other healthcare professionals have the responsibility to educate their patients to help prevent and treat the flu. With peak flu season upon us, we wanted to share common questions and challenges that healthcare professionals need to address.
How do I prevent the flu?
One of the most common questions healthcare professionals get is if the flu can be prevented. While the flu virus is always pervasive and widespread it is possible to prevent the flu.
Basic hygiene is the common sense defense against most microorganisms. Young children need extra guidance to develop long-term hygiene habits. It’s A Snap is a great resource for teachers and nurses to instill the habit of handwashing. Raising Children an Australian parenting website has good resources for parents to teach hygiene habits to their kids.
However, the flu vaccine is the best bet against the flu virus. Healthcare professionals are urged to make a strong recommendation for the flu vaccine to their patients.
Do I really need the flu shot?
Young children and older adults have weaker immune systems. They are more susceptible to the flu virus. Chronic medical conditions like asthma, cancer, diabetes, obesity, cystic fibrosis, HIV/AIDS, Kidney or liver disease also make people vulnerable to the flu. Pregnant women are also at a higher risk.
If your patient is in a high-risk group, strongly encourage them to get the flu shot. However, the CDC recommends everyone over the age of 6 months get vaccinated. Healthcare professionals should advise all patients to get the flu shot.
Most adults know the importance of vaccines for themselves and their loved ones. They just need reminders and encouragement from healthcare providers to make the time. Make a recommendation and follow up to ensure that the patient has received their vaccine.
I am unsure about the flu vaccine!
Vaccine advocacy is not easy. Sometimes it can be a difficult conversation. Patients can have valid fears and concerns. The CDC recommends the “SHARE” method to help patients make informed decisions about the flu vaccine.
- Share the reasons to get vaccinate. Focus on the patient’s age, lifestyle, health and risk factors.
- Highlight Positive experiences. Draw from your experience as appropriate to showcase the benefits and assuage any fears.
- Address patient questions. Listen to your patient’s questions and concerns. Answer them in easy to understand language and show empathy.
- Remind patients that flu vaccines protect them and their loved ones from flu and flu-related complications.
- Explain the potential costs of getting the flu. Make them aware of health effects and financial costs. Remind them that the flu can result in missed work and family obligations.
The CDC has toolkits to help healthcare professionals have these conversations. It includes email templates, flyers, and talking points tailored to patient age.
https://www.youtube.com/watch?v=QvyaE_eXDJU&t=1s
I don’t want the flu shot!
Healthcare professionals do not have a responsibility to ‘convince’ their patients to take the flu shot. Your responsibility is to provide them with all the facts (pros and cons) so that they can make an informed decision.
There will always be patients who do not want to take the flu vaccine. “SHARE” the information but respect their autonomy. Some patients may have additional fears and questions about the flu vaccine. The American Association of Family Physicians suggests the “Ask-Tell-Ask” approach to address questions and fears.
Their method recommends a physician and nurse pair working together. However, any healthcare professional can use this framework to address concerns.
- Ask – Ask why they do not want or are hesitant about the flu shot. Request their permission to share more information.
- Tell – Provide them the facts and data relevant to their concern.
- Ask – Ask for their thoughts about the flu vaccine. Administer the vaccine if they want one. Respect their decision if they don’t but welcome conversation.
I am worried about ____
When you use the ask-tell-ask framework, patients will share a wide variety of concerns. Here are some common concerns you may encounter and possible responses.
- I’ll get sick/Someone I know got sick after taking the flu shot: The flu vaccine does not contain a live virus. It will not give you the flu. Some people may feel tired or weak while their immune system builds antibodies.
- The flu shot is not effective: Flu vaccines vary in efficacy every year. However, studies have shown that the flu vaccine can reduce the risk of flu by 40-60%. Many people do not get the flu after being vaccinated. 1 Some protection is better than none. Those who get the vaccine have shorter and milder flu, reduced ICU admission and durations.2
- I am healthy: The CDC recommends everyone over 6 months to be vaccinated. Even healthy people get the flu. You can risk symptoms like high fever, body aches, nausea, vomiting, and diarrhea. You risk missing days at work or missing out on family events. Healthy people who get the flu may severely risk vulnerable loved ones.
- I got a flu shot last year: The flu virus mutates rapidly. Every season has a different strain of the virus. The flu vaccine is specifically designed to target the dominant strains during the current flu season.
- The flu is just a bad common cold: Apart from a runny nose, congestion, and sneezing the flu can have other symptoms like fever, chills, fatigue, diarrhea, sore throat and more. Unlike the cold, severe flu can also result in death.
- I am worried about a reaction: People who have the rare Guillain-Barré cannot take the flu vaccination. However, the flu vaccine is safe for most people. People who have egg allergies should talk to their doctor. Doctors may be able to provide a vaccine without egg proteins or manage the allergic reactions. However, if someone has had a serious reaction to previous flu vaccine may need to avoid the vaccine.
After addressing their concerns, some patients may still not want the vaccine. Respect their decision and encourage further conversations to learn more about the vaccine.
I have the flu. What should I do?
The flu virus spreads rapidly and easily. Despite proper hygiene and precautions like vaccination, many people can get the flu.
If a patient has the flu, strongly encourage them to stay at home until they recover, unless they require medical care. Most healthy adults can manage the flu at home. Many healthcare providers offer virtual or phone consultations. This way patients avoid contact with others and transmitting the virus, especially in places with vulnerable populations like hospitals and clinics.
Patients can still be contagious after they feel better. It is recommended they wait at least 24 hours after the fever goes away before going out again.
When at home recovering, patients should get plenty of rest and have plenty of liquids. Consuming plenty of soup and water are essential if they are at risk of dehydration due to diarrhea. Many may need to take a break from their exercise routines and rest. Advise them to listen to their body and not overwork themselves. Most traditional home remedies like chicken soup, lozenges, warm compresses, sinus rinses, and steam inhalation can help reduce symptoms. Consult with the patient and direct them to the appropriate over the counter (OTC) medication to relieve their specific flu symptoms (pain/fever reducer, decongestant, expectorant, suppressants).
Occasionally, some patients may need prescription medications to relieve their symptoms. Use your best judgment and experience to prescribe the dosage and medication that works for them. If necessary prescribe antivirals (oseltamivir, zanamivir, peramivir) to treat the flu. Some flu strains are resistant to some antivirals, so check with the CDC and other trade publications to see which are recommended for this season’s strains.
How long does the flu last? How long will I be sick? How many days will I miss work/school?
A bout of the flu typically lasts one to two weeks, with severe symptoms subsiding in two to three days. However, weakness, fatigue, dry cough, and a reduced ability to exercise can linger for three to seven days.
How long am I contagious?
After symptoms start, adults can spread the virus for five to 10 days. However, the amount of virus spread decreases significantly after three to five days. Adults are most contagious with the flu from 24 hours before symptoms start to three to five days afterward.
I am really sick. Can you please prescribe me some antibiotics?
Many patients will have severe flu symptoms that cannot be alleviated by traditional home remedies or OTC medication. They will need prescription medication and even hospitalization to treat the flu. However, antibiotics are ineffective against the flu. Antibiotics are designed to combat bacteria and do nothing against viruses like the flu.
Many patients confuse antivirals with antibiotics. Explain the difference to them. The CDC has a helpful chart to help understand the differences between bacterial and viral infections. 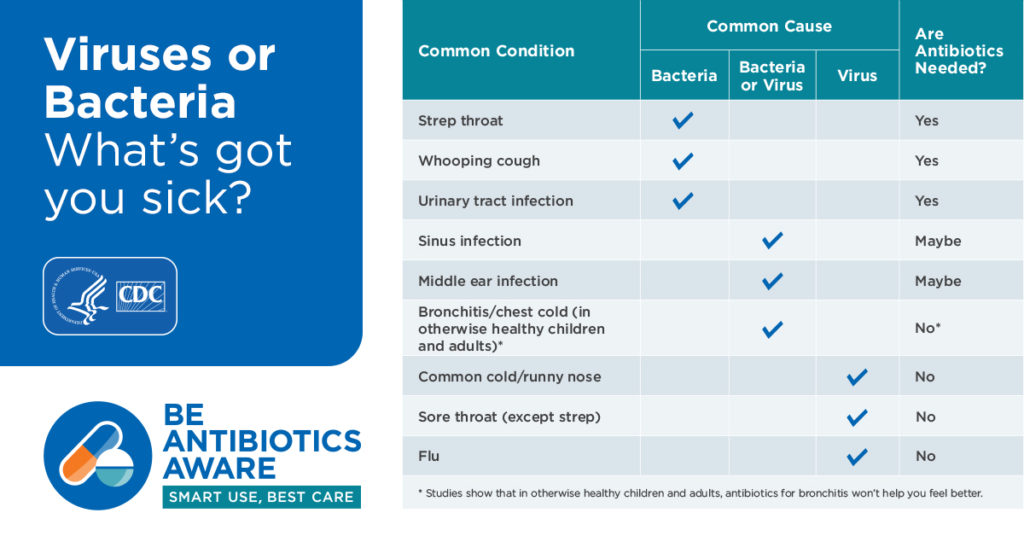
Advise them that viruses need to run their course. The best thing they can do is rest and let time ease their symptoms. However, listen to their concerns and offer antivirals and other prescription medication for their symptoms if needed.
Some of your patients may be concerned that they have strep throat, pertussis (whooping cough) or a respiratory tract infection rather than the flu. Some of these infections, like strep throat, are very common, especially with young children. Simple swab tests can confirm the diagnosis. If you or the patient believe that some of the symptoms may be related to a bacterial infection, get a rapid test done and act accordingly.
Resources
We hope you have the information you need to address all your patient questions and needs this flu season. The CDC and your local Department of Health Services also contain a wealth of resources for patient care including seasonal/local information, guides for talking to patients, printable resources for your practice, and email templates.
Our self-paced online course on “Developing Effective Communication Skills” helps pharmacists and healthcare professionals improve patient communications.
References:
Vaccine Effectiveness Studies – https://www.cdc.gov/flu/professionals/vaccination/effectiveness-studies.htm
Arriola C, Garg S, Anderson EJ, Ryan PA, George A, Zansky SM, Bennett N, Reingold A, Bargsten M, Miller L, Yousey-Hindes K, Tatham L, Bohm SR, Lynfield R, Thomas A, Lindegren ML, Scahffner W, Fry AM, Chaves SS, Influenza Vaccine Modifies Disease Severilty Among Community-dwelling Adults Hospitalized with Influenza – https://www.ncbi.nlm.nih.gov/pubmed/28525597
