Choosing between food and insulin – is the cost of diabetes care sustainable?
Recently the news is inundated with stories about insulin costs and the difficulties that patients with diabetes face. Some patients have stopped taking insulin altogether or reduced how often they take insulin. This leads to adverse effects on their health and wellbeing. Sometimes the outcomes can be fatal. Affordability of care has made the healthcare professional’s role in the care of the patient with diabetes even more challenging.
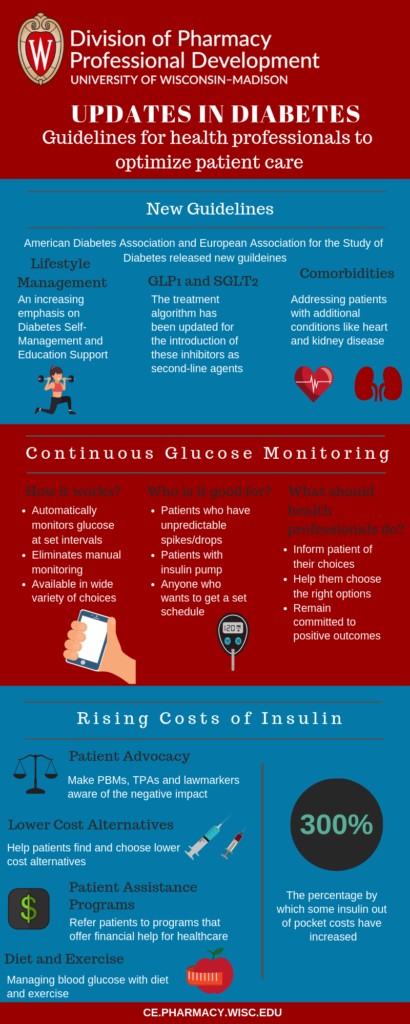
While the outlook is bleak in relation to insulin costs, there have been exciting developments in the treatment of diabetes. These developments are improving and enhancing the way healthcare professionals can help their patients manage diabetes. The American Diabetes Association (ADA) and European Association for the Study of Diabetes (EASD) recently released new guidelines in the treatment of Type 2 Diabetes. Another recent development is the growth of Continuous Glucose Monitoring Systems (CGMS). These systems have come a long way and have the potential to be a care standard in the near future.
This blog will update healthcare professionals on the latest developments in the treatment and management of diabetes. We will highlight the new guidelines and explore the benefits of CGMS. Finally, we will discuss the impact of insulin cost and explore options for healthcare professionals to help their patients struggling to afford insulin.
New Guidelines for the Management of Type 2 Diabetes
 The ADA and EASD published position statements on the treatment of diabetes in 2012 and 2015. These organizations regularly convene a panel to discuss the latest research and updates in the treatment of type 2 diabetes. They publish new guidelines whenever there is compelling data to update treatment positions. The most recent panel convened in 2018 and published their Consensus Report in October 2018.
The ADA and EASD published position statements on the treatment of diabetes in 2012 and 2015. These organizations regularly convene a panel to discuss the latest research and updates in the treatment of type 2 diabetes. They publish new guidelines whenever there is compelling data to update treatment positions. The most recent panel convened in 2018 and published their Consensus Report in October 2018.
There are a number of substantial revisions in addition to three areas of focus within the new guidelines: lifestyle management, update in administration of sodium–glucose cotransporter 2 (SGLT2) inhibitor or a glucagon-like peptide 1 (GLP-1) receptor agonist agents, and considerations for comorbidities like cardiovascular disease, chronic kidney disease, or clinical heart failure.
Lifestyle Management
Data shows that Diabetes Self-Management and Education Support (DSMES) plays a significant role in the management of diabetes. DSMES programs have shown a positive impact on medication adherence, healthy eating, and physical activity. This has been especially critical for patients with obesity to meet targeted weight loss.
The panel concluded that all patients with type 2 diabetes should be given access to ongoing DSMES programs. These programs are usually face-to-face contact in either one-on-one or group settings. DSMES teams usually include a registered nurse, a dietician/nutritionist, and a pharmacist or certified diabetes educator.
For patients who are taking glucose-lowering medication, there is an emphasis on adherence. The DSMES team works with the patient to ensure that medications are taken on time, are yielding desired results, and not affecting negatively with any other medication.
GLP-1 and SGLT2
The treatment algorithm based primarily on demonstrated cardiovascular risk reduction on specific patient populations have elevated the use of GLP-1 and SGLT2 as second-line agents behind and in conjunction with metformin. We recommend providers and patients discuss treatment objectives and optimal therapy that means the needs of each patient.
Comorbidities
Patients with diabetes can have a wide number of comorbidities. The new guidelines focus on
- Clinical Cardiovascular Disease (CCD)
- Chronic Kidney Disease (CKD)
- Clinical Heart Failure (CHF)
- Atherosclerotic cardiovascular disease (ASCVD)
For patients with CCD a sodium-glucose cotransporter 2 (SGLT2) inhibitor or a glucagon-like peptide 1 (GLP-1) receptor agonist with proven cardiovascular benefit is recommended.
If patients have CKD, CHF, of ASCVD an SGLT2 inhibitor with cardiovascular benefit is recommended while GLP-1 receptor agonists are recommended as the first injectable.
These guidelines are a shift from the traditional use of metformin and either supplement or replace it in early treatment phases based on patient characteristics.
In addition, regular follow-ups every 3-6 months are recommended to reassess and modify treatment in order to avoid clinical inertia. The Hemoglobin A1c (HbA1c) levels during these assessments provide further guidance for medication.
What do the guidelines mean for healthcare professionals?
The emphasis on DSMES puts forth a strong case for interprofessional education and collaboration. Nurses, doctors, pharmacists, dieticians/nutritionists, and diabetes educators have to collaborate and work together to improve the health outcomes for patients with diabetes. Patients will need referrals and follow-ups to ensure that they are getting the right tools and support for self-management. Healthcare professionals will also need to further develop their communication skills to better educate their patients about diabetes.
Healthcare professionals will need to identify patients with comorbidities as recommended by the guidelines and determine if any medication updates are necessary. Doctor and pharmacist teams will need to communicate with patients so that they understand the changes in medication and adhere to them.
Continuous Glucose Monitoring Systems
Almost everyone is familiar with glucose test strips and meters. Patients with diabetes are all too familiar with the routine prick to draw blood samples to test for glucose. Even those without diabetes know this routine. However, glucose testing has come a long way over the past few years. CGMS offers a viable alternative from traditional glucose testing.
What is CGMS and how is it different?
As the name suggests CGMS can monitor glucose levels continuously. Patients no longer need to schedule a time and remember to test their glucose. The CGMS device automatically tests glucose at 1, 5, 10, or 15-minute intervals. Patients who manually monitor their glucose are often susceptible to sudden spikes or drops in their glucose levels. However, CGMS can notify patients of these spikes/drops preemptively and allow them to take precautions.
There are many options for CGMS. Sensors can be placed under the belly or at the back of the arm. Readings can be sent to a monitoring device or to a smartphone app depending on the type of CGMS. Many modern CGMS allow patients to download their data and get a better understanding of their glucose levels and trends.
Who are the optimal patients for CGMS?
Patients who have variable glucose levels, who experience frequent spikes/drops, or who are unable to meet their A1C goal maybe benefit from a CGMS. Data from CGMS can help healthcare professionals and patients work together to improve the diabetes care plan.
CGMS also works well paired with insulin pumps. Insulin pumps deliver insulin all day through a catheter placed under the skin. In addition to base rates, patients can press a button to deliver a bolus dose whenever they have a meal. A CGMS paired with an insulin pump can take the guesswork out of basal and bolus doses and deliver insulin based on real-time glucose levels.
Implications for healthcare professionals
CGMS can eliminate uncertainty by preventing missed and forgotten readings. By providing a wide range of valuable glucose data CGMS can help inform medication and dosage decisions. In light of the new guidelines, CGMS can help DSMES be more informative and robust. It can also help healthcare professionals inform dosage decisions in case of comorbidities.
However, there are many limitations to CGMS. It may not be best suited or valuable for all patients. Many patients will have cost prohibitions that limit the type of CGMS. Some patients may also find CGMS invasive and obtrusive. Healthcare professionals have a responsibility to be well informed about CGMS and available options. They should work with their patients to determine if CGMS is right for them and if so what type of CGMS (cost, placement, device connectivity) would serve the patient best.
Rising Out of Pocket Cost of Insulin
Perhaps the greatest challenge in the care of patients with diabetes is rising out of pocket cost of insulin. Recent news reports have cited that some insulin costs have increased by 300%. When patients are being forced to choose between their next meal and insulin, it becomes difficult for the healthcare professional to address guidelines such as medication adherence or dosage adjustments.
Patient choices related to insulin not only impact their diabetes but also any other comorbidities they may have. Varying glucose levels due to improper schedules of insulin can even rule out CGMS and other technology as viable management options. The general consensus within the healthcare community is that the rising costs of insulin are unsustainable.
However, there are a few things healthcare professionals can do to help their patients manage rising out of pocket costs.
Patient Advocacy
The greatest impact healthcare professionals can have for their patients is to be an outspoken advocate. Healthcare professionals can educate and influence Pharmacy Benefit Managers (PBMs) and Third-Party Administrators (TPAs) about the negative impacts and long term consequences of rising out of pocket costs.
A major factor impacting the rising out of pocket costs is the way rebates are structured. Prescription drug manufacturers offer rebates on their products, but the discount is not often passed down to patients. Lawmakers have proposed changes to this structure so that patients can benefit from rebates and see lower drug costs, especially in the case of vital drugs like insulin. Healthcare professionals can contact lawmakers and advocate for laws that provide optimum patient outcomes.
Lower Cost Alternatives
Doctors and pharmacists can work together to find lower-cost alternatives. Although biosimilars have not fulfilled their lower cost potential, there are biosimilar alternatives to insulin that may be available at a lower cost. Some retailers also sell over the counter insulin analogs that may be suitable for some patients.
Insulin analogs and biosimilars may not be suitable for all patients and conditions. Care teams will have to work with the patient and monitor their progress to ensure that there are no adverse effects of the alternative.
| [panel type=”info” heading=”UPDATE” ] On March 4th 2019, Eli Lilly announced that they will be introducing half-priced generic insulin alternative to Humalog. The discussion continues if these lower cost alternatives are actually affordable. CNN[/panel] |
Prescription Assistance Programs
Prescription Assistance Programs (PAPs) offer assistance to people who lack prescription coverage or cannot afford medication. These programs are run by a wide range of organizations including drug companies, patient advocacy groups, non-profits, and local clinics. They are often able to provide free to low cost prescriptions to qualifying individuals.
Healthcare professionals should have awareness of various PAPs available in their area. They must communicate regularly with their customers to identify any challenges they have with affording medication and refer them to PAPs that may be able to help.
Diet and Exercise
Diet and exercise are never a replacement for necessary prescription medication. However, they can help minimize the negative impact of improper insulin schedules. Low glycemic diets combined with food diaries and glucose tracking can help patients make smart food choices. DSMES teams can work with patients to track food and health activities to manage diabetes.
In addition, healthcare teams can ensure that patients take advantage of all resources that are available and affordable with their current insurance. They can follow up with patients to ensure that they are checking in with their primary care provider or endocrinologist. This allows doctors to adjust doses and medication as needed based on what the patient can afford.
The Healthcare Professionals Role in Management of the Patient with Diabetes
Diabetes treatment options, medications, and technology are always changing. Continued research and data collection has informed several new treatment guidelines over the years. CGMS combined with smart apps has made it easier to monitor glucose as well as nutrition and exercise.
While these innovations have improved patient care, current laws and the structure of rebate programs is making insulin unaffordable to many.
Healthcare professionals have a lot to keep up with to help their patients with diabetes. The 2019 Madison Clinical Conference is focused on the management of patients with diabetes. Pharmacists and nurses will have the opportunity to interact in an interprofessional environment and learn more about the latest updates in diabetes care including new guidelines, CGMS, insulin pumps, nutrition, and more. We have put together an excellent line up of expert faculty presenters and will have six interactive workshops to choose from on day 2. You will also have an opportunity to network with other professionals and discuss solutions for issues such as rising costs.
References:
http://care.diabetesjournals.org/content/diacare/early/2018/09/27/dci18-0033.full.pdf
https://www.cdc.gov/diabetes/dsmes-toolkit/index.html
https://www.webmd.com/diabetes/guide/continuous-glucose-monitoring#1
https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/InVitroDiagnostics/GlucoseTestingDevices/default.htm
http://care.diabetesjournals.org/content/40/12/1614
http://www.diabetes.org/living-with-diabetes/treatment-and-care/medication/insulin/how-do-insulin-pumps-work.html
